Ulcerative Colitis IDB: A Comprehensive Guide

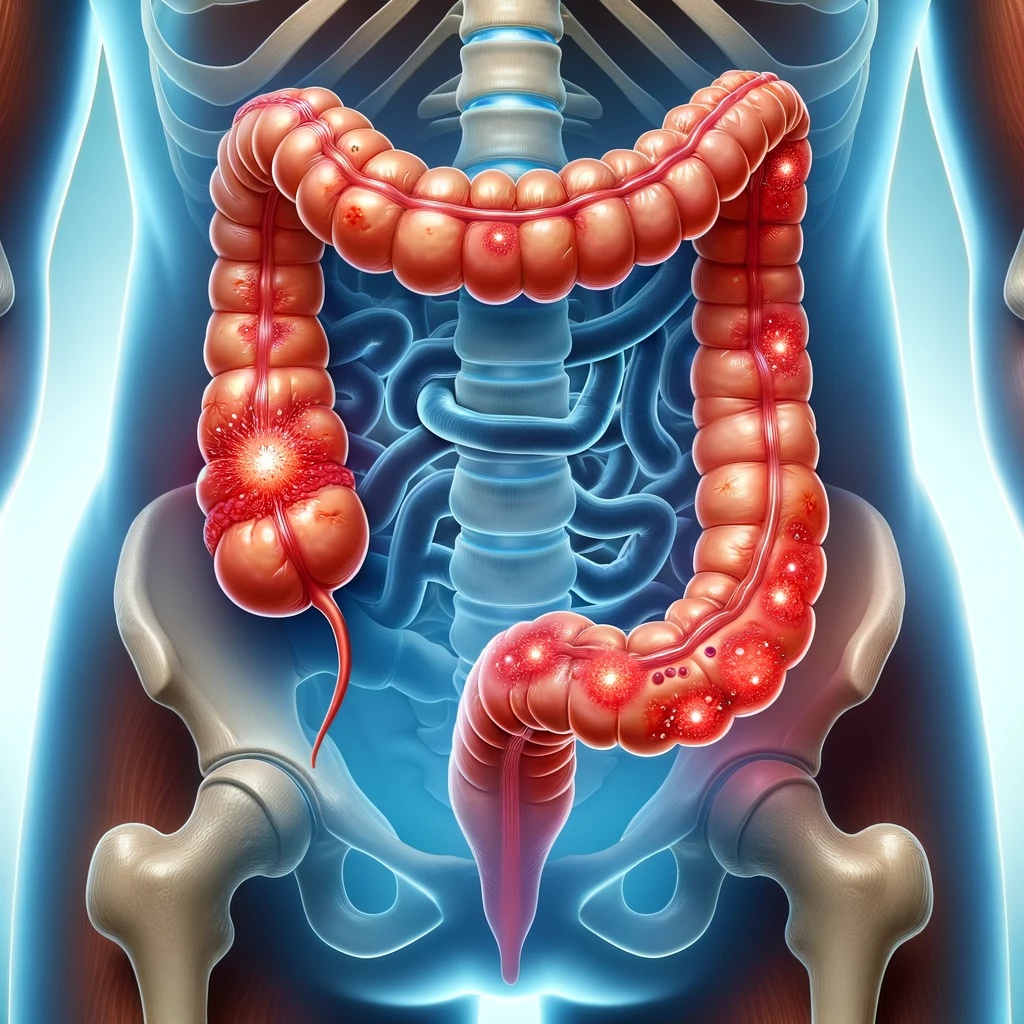
Ulcerative colitis IDB (UC) is a chronic condition that causes inflammation and ulcers in the lining of the large intestine (colon) and rectum. It falls under the category of inflammatory bowel diseases (IBD), not to be confused with irritable bowel syndrome (IBS), a different condition. UC is a long-term condition that can have a significant impact on the quality of life of those affected.
What is Ulcerative Colitis IDB?
Ulcerative colitis IDB is characterized by the inflammation of the innermost lining of the colon and rectum. This inflammation typically leads to the development of sores or ulcers. Unlike Crohn’s disease, another type of IBD that can affect any part of the gastrointestinal (GI) tract, UC is limited to the colon and rectum.
Causes and Risk Factors
The exact cause of UC is unknown, but it’s believed to result from an abnormal response of the immune system. Normally, the immune system defends against pathogens, but in UC, the immune system mistakes food, beneficial gut bacteria, and the cells lining the colon as foreign invaders, leading to chronic inflammation.
Several factors may increase the risk of developing UC:
- Genetic Factors: A family history of UC increases the risk.
- Environmental Factors: Diet, air pollution, and hygiene practices may play a role.
- Age: It often begins before the age of 30.
- Ethnicity: More common in certain ethnic groups.
Symptoms of Ulcerative Colitis IDB
The severity of symptoms can vary and may include:
- Diarrhea: Often mixed with blood or pus.
- Abdominal Pain: Cramping and discomfort.
- Urgency to Defecate: Frequent, often urgent bowel movements.
- Fatigue: A common complaint due to inflammation and anemia.
- Weight Loss: Due to reduced appetite and nutrient absorption.
Diagnosing Ulcerative Colitis IDB
Diagnosing UC involves a combination of tests and procedures:
- Blood Tests: To check for anemia or infection.
- Stool Sample: To rule out infections.
- Colonoscopy: Provides a visual of the entire colon.
- Biopsy: Tissue samples taken during colonoscopy for detailed examination.
Treatment Options
Treatment for UC aims to reduce the inflammation, manage symptoms, and induce and maintain remission:
- Medication: Anti-inflammatory drugs, immune system suppressors, and biologics.
- Surgery: In severe cases, removing the entire colon and rectum (proctocolectomy) may be necessary.
- Nutritional Support: Diet modifications and supplements.
Lifestyle Management and Diet

Living with UC means making lifestyle adjustments:
- Dietary Changes: Avoiding foods that trigger symptoms.
- Stress Management: Stress can aggravate symptoms.
- Regular Exercise: Helps with overall health.
Complications
Potential complications include:
- Colon Cancer: Regular screenings are recommended.
- Primary Sclerosing Cholangitis: A liver condition linked with IBD.
- Severe Dehydration: Due to diarrhea.
Current Research and Future Directions
Researchers are exploring new treatments, including stem cell therapy and microbiome manipulation. Understanding the genetic and environmental factors that contribute to UC is also a significant area of research.
Conclusion
Ulcerative colitis IDB is a challenging condition, but with proper treatment and lifestyle adjustments, individuals can manage their symptoms and maintain a good quality of life. Ongoing research continues to improve our understanding and treatment of this complex condition.
Related Articles
About the Author




0 Comments